MissionLiFE
August 27, 2024
[ad_1]

1. Introduction
Covid-19 in Belgium caused increased incidence of premature deaths, especially in vulnerable population groups such as the elderly and persons suffering from cardiovascular disease [1]. This is a cause of concern, given that climate change projections indicate a significant rise in the frequency, duration, and intensity of extreme heat episodes. Even if the goals of the Paris Agreement to avoid dangerous
climate change are achieved, a substantial rise in the frequency of deadly heat episodes is still expected [2].
In temperate climate zones, heatwaves cause more fatalities than any other weather-related disaster [3]. A notable example stems from the comparison between Hurricane Katrina in 2005, which resulted in approximately 1500 deaths [4], and the 2003 European heatwave, which led to 70,000 reported deaths [5]. Additionally, the combined death toll from the 2003 European heatwave and the 2010 Russian mega-heatwave accounted for over 80% of all deaths caused by natural disasters in Europe between 1970 and 2012 [6]. The heat-related mortality burden during the summer of 2022, the hottest season on record in Europe, has been estimated at 62,000 [7].
In July 2024, the UN Secretary General issued a call to action on extreme heat [8], underlining the urgency of the problem, among other posing severe risks to health and economic stability worldwide. The statement highlighted the need to protect those most affected by extreme heat, such as children, the urban poor, and outdoor workers; and called to boosting resilience using data and science.
City dwellers face a heightened risk of mortality from extreme heat [9,10,11]. Cities experience air temperatures in excess of rural values, especially at night, temperatures being higher by up to 7–8 °C and more. In an analysis covering Belgian cities [12], it has been found that urban areas experience twice as many heatwave days as their rural surroundings. In addition, there is evidence [13] that the urban heat island intensity itself may increase during heatwaves. While some of the increased urban mortality can be attributed to the vulnerability of urban populations, such as a higher proportion of isolated elderly individuals, it is also directly linked to the urban heat island (UHI) effect itself [14].
The mortality impact of heatwaves is often downplayed by citing the ‘harvesting’ phenomenon, where frail individuals die a few days or weeks earlier than they would have otherwise. However, this effect diminishes with stronger heatwaves. For instance, during the 2003 European heatwave, the harvesting effect was modest [15]. Overall, the number of life years remaining at death from heat-related causes has been estimated at approximately eight years [16,17].
The monetary cost of heat-related mortality is typically calculated by invoking the Value of a Statistical Life (VSL), which is an individual willingness to pay for a reduced mortality risk [18]. For example, if a survey reveals that individuals are willing to pay EUR 30 to reduce their risk of dying by one in 100,000, then the total willingness to pay would be EUR 3,000,000 (EUR 30 × 100,000). This amount represents the VSL, which in this case is EUR 3,000,000. Hence, the VSL is not the value of a specific individual’s life, but rather an aggregation of individual values for small changes in the risk of death.
From this definition, it should be clear that the VSL constitutes a highly subjective metric, being fraught with substantial uncertainty. For instance, VSL estimates across the US and Europe range from EUR 1 million to EUR 10 million [19]. Use of the VSL in the context of heat-related mortality has raised concern, considering that, often, this quantity has been established in the context of, e.g., transportation accident risks, which is very different from the mortality risks associated with heat exposure [20]. In particular, economic assessments using the Value of a Statistical Life (VSL) do not explicitly account for age, thus assuming that life expectancy at the time of death is similar across all mortality causes. However, temperature–mortality relationships indicate that heat exposure disproportionately affects older populations [11]. Some have questioned the validity of using VSL in heat-related mortality, stating that “the literature offers no heatwave-specific willingness to pay” [21], or that “the use of the VSL can be controversial” [22].
Hence, while a deeper understanding of the economic impacts of
climate change on health is necessary to alert decision makers to the urgency of mitigation and to support concrete adaptation actions [21], and while the cost of heat-related mortality often dominates economic assessments of
climate change impacts [23], there remains a significant level of uncertainty in determining the monetary value to be assigned to a human life.
In the present paper, we attempt to estimate the monetary cost attributed to heat-related mortality in an objective manner, by leveraging the reported economic impact of measures put in place to contain mortality during the first wave of the COVID-19 pandemic in Belgium. Concretely, the cost of avoided mortality is estimated by equating the following: (1) the welfare loss incurred during the first wave of the pandemic (March–June 2020), using gross domestic product (GDP) as a metric; (2) the estimated number of averted deaths during the same period, owing to the measures that were implemented by the government to contain the pandemic.
2. Data and Methods
2.1. COVID-19 Mortality as a Proxy for Heat-Related Mortality
Before estimating GDP loss and the associated avoided mortality, the validity of employing COVID-19 mortality as a basis for establishing heat-related mortality costs is assessed, questioning whether COVID-19 mortality serves as an adequate proxy for heat-related mortality.
The available evidence seems to indicate that it does. The health profile of people vulnerable to severe COVID-19 is very similar to that of people who are sensitive to (and die from) excessive heat [24], including the following populations:
- Elderly individuals, especially those with multiple chronic conditions and those living in nursing homes;
- People with underlying medical conditions such as cardiovascular and cerebrovascular disease, hypertension, chronic pulmonary disease, kidney disease, diabetes, obesity, Alzheimer’s disease, and dementia;
- Socially isolated persons (homeless people, migrants, older people living alone).
In addition, the expected remaining lifetime at the time of death is highly similar for heat- and COVID-19-related mortality, amounting to 7.7 years for COVID-19 [25] versus 8 years for heat-related mortality [16,17].
Considering the above elements, it is fair to say that many of the risk factors for severe COVID-19 overlap with those for heat-related mortality. Therefore, COVID-19 mortality appears to constitute a reasonable proxy for heat-related mortality.
2.2. Gross Domestic Product (GDP)
In Belgium, the first wave of the pandemic lasted from March to June 2020, leading to the largest decline in economic output since World War II. This decline was mainly related to the containment measures put in place by the government, drastically reducing the transmission of infections within the population. Starting on 14 March 2020, Belgium enforced a nationwide lockdown, closing schools, universities, restaurants, cafes, gyms, and non-essential businesses. Mobility was heavily restricted, and public gatherings were banned. These measures were gradually eased beginning 4 May 2020, allowing a phased return to social and economic activities. Note that only non-pharmaceutical measures were involved, as vaccination campaigns only began in 2021.
Gross domestic product (GDP) measures the value of all final goods and services produced within a country in a given year. Alternatively, it can be considered as the total income earned by households and businesses in a year [26]. A decline in GDP indicates a reduction in economic activity and is associated with job losses, reduced working hours, lower wages, and overall lower income levels for businesses and individuals. All these factors constitute a direct cost to the community.
In Belgium, quarterly GDP is published by the National Bank of Belgium [27]. Their estimates are based on national and regional accounts, which are compiled according to the requirements of the European System of Accounts (ESA 2010) [28], which is an internationally compatible EU accounting framework for a systematic and detailed description of an economy.
Table 1 presents reported GDP values for quarters 1 and 2, as well as their sum, for recent years. The consideration of only the first two quarters relates to the fact that the paper focuses on the first COVID-19 wave, which occurred between March and June 2020, i.e., within quarters 1 and 2 of that year.
2.3. COVID-19 Mortality
In early March 2020, the Belgian health institute Sciensano was mandated by the regional and federal authorities with the task to gather daily nationwide COVID-19 mortality figures [29]. Considering that the standard registration procedure of the specific causes of death is a rather slow process, an ad hoc surveillance was established to allow the near-real-time monitoring of COVID-19 mortality. A centralized data registration was established, gathering data from hospitals, long-term health care facilities, and general practitioners.
Death reporting was exhaustive, including all deaths potentially attributable to the pandemic, irrespective of the diagnostic method and setting. Subsequent studies showed that the ratio between observed overall excess mortality and reported COVID-19 mortality was remarkably close to unity in Belgium [30,31,32,33]. This consistent reporting of comprehensive and reliable mortality figures makes the Belgian data particularly suitable for use in quantitative studies as the one presented here.
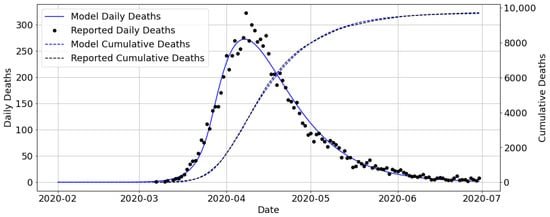
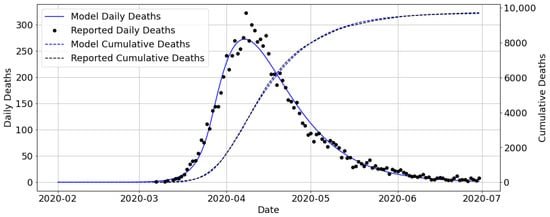
Daily mortality data of the first COVID-19 wave in Belgium (March–June 2020) were acquired from the dashboard managed by Sciensano [34]. The total number of reported COVID-19 deaths over this period amounted to 9721 (Figure 1).
2.4. Epidemiological Modelling
One of the main challenges of the approach presented here is the estimation of the hypothetical number of avoided deaths that would have occurred in the absence of any containment measures. Apart from adopting insights from the literature, we will apply an epidemiological model to evaluate scenarios of pandemic containment, in particular scenarios based on measures taken by individuals at a modest or no economic cost, as opposed to the nationwide lockdown imposed by the government.
The epidemiological model used here to simulate the evolution of the pandemic and to assess the potential number of averted deaths is the compartmental model developed by De Visscher [35]. This model simulates the time evolution of the number of uninfected (U
), infected (
I
), sick (
S
), very sick (
V
), better (
B
), recovered (
R
), and deceased (
D
) individuals. In the remainder of this paper the ‘better’ and ‘recovered’ categories will be disregarded as our focus is on mortality only and considering that the omission of these categories has no bearing on mortality outcomes.
The model is based on the following system of coupled ordinary differential equations (an overhead dot denoting a time derivative):
In these equations, the total population (P
) is set at 11.5 million, the total Belgian population in early 2020. The symbols
r
1
,
…
,
r
6
shown between brackets refer to the transfer rates between compartments, as graphically shown in Figure 2. The coefficients
k
2
,
⋯
,
k
6
are fixed to values that represent COVID-19 characteristics [35], such as the incubation time. The coefficient
k
1
holds a central position, being related to the reproduction number (see above) through
R
0
≈
a
k
11
, with
a
≈
10
days
(the units of
k
11
being days−1). Unlike the other coefficients, it is an adjustable parameter in the model.
The model contains a mechanism to simulate the impact of measures aiming to reduce
R
0
,
by introducing an effectiveness
E
,
with
R
0
,
after
=
1
−
E
R
0
,
before
;
the subscripts refer to the reproduction number before and after the introduction of a measure, such as a lockdown. A measure that is 100% effective (
E
=
1
) would bring
R
0
to zero, effectively terminating the spread of the virus. A measure with an effectiveness of 0% corresponds to a situation without any mitigating measures at all.
The system of ordinary differential Equations (1)−(5) is solved using Runge–Kutta–Fehlberg (RKF45) integration over the period from 1 February to 30 June 2020. The coefficientsR
0
and
E
were adjusted until the model yielded a satisfactory match with daily number of deaths observed in Belgium (Figure 1), resulting in
R
0
=
3
and
E
=
0.91
. The value obtained for the reproduction number
R
0
matches nicely with independent estimates of
R
0
≈
2.9
[36]. The infection fatality rate (IFR), having a default value in the model of 1.5%, was kept as this value coincides well with reported values for Belgium of 1.47% [32] and 1.251−1.672% [37].
With these parameter values, the modelled cumulative number of deaths matches the reported number within 0.5% (Figure 1). The time tendencies simulated for the various model compartments using these calibrated parameters are shown for Belgium for February−June 2020 in Figure 3.
The conclusion of this subsection is that the model is capable of correctly reproducing daily and accumulated deaths in the period February−June 2020, including the effect of the lockdown (through the parameterE
). More details regarding the model and its applications are available in the paper by De Visscher [35].
4. Discussion
The monetary value assigned to a human life in this study, estimated at EUR 377,000 ± EUR 222,000, stands in stark contrast to the Value of a Statistical Life (VSL) typically cited in the literature, which ranges between EUR 1 million and EUR 10 million [19] (see the Introduction Section).
This discrepancy is not unexpected given the fundamentally different constructs these values represent. While the VSL is derived from willingness-to-pay (WTP) studies that assess how much individuals are willing to pay to reduce their risk of dying, our estimate is based on actual economic losses incurred during the COVID-19 pandemic. The VSL method aggregates individual preferences across small changes in mortality risk, often in contexts like transportation accidents, which involve different demographic profiles and risk perceptions than those associated with heat-related mortality [22,44].
Moreover, the VSL does not explicitly account for age, instead assuming a uniform life expectancy across all causes of death. However, empirical evidence consistently shows that heat exposure disproportionately affects older populations, who have fewer remaining life years at the time of death [11]. This assumption introduces a significant bias when applying VSL to heat-related mortality, where the affected demographic group primarily consists of the elderly. As such, using VSL in this context can lead to overestimation of the economic value of avoided deaths.
Our study’s estimate aligns more closely with the Value of a Life Year (VOLY), which is designed to account for the remaining life expectancy at the time of death. When we divide our estimate of EUR 377,000 ± EUR 222,000 by the average remaining life years (approximately eight years for heat-related deaths), the resulting VOLY of EUR 47,000 ± EUR 28,000 falls within the range recommended for European countries (EUR 25,000–EUR 100,000) [44]. This suggests that VOLY may be a more appropriate metric for valuing lives in the context of climate-related mortality, particularly for older populations.
Furthermore, the significant disparity between VSL and VOLY observed here echoes findings in the broader literature, where differences of up to an order of magnitude have been reported [45,46]. Such disparities underscore the inherent uncertainties in these metrics and the importance of context-specific valuation methods. One study noted that relying on VSL can lead to substantially higher estimates compared to VOLY, especially when applied to scenarios involving predominantly older individuals [17], concluding that “this is a major and far from resolved source of uncertainty in economic terms”. Our analysis, therefore, suggests that VOLY should be the preferred approach for economic evaluations of heat-related mortality, given its closer alignment with the actual demographic characteristics of the affected population.
It is insightful to apply the monetary value assigned to human life to estimates of projected future heat-related mortality. Currently, average heat-related mortality in Belgium stands at approximately 70 excess deaths per year (reference period 1980–2010). Future projections estimate that the annual average of heat-related deaths could increase to around 2800 by the end of the century under a high climate scenario (2837 annual deaths under RCP8.5 are cited in [23] and 2777 annual deaths under SSP5-8.5 in [47]). Multiplying this projected figure of 2800 annual deaths by the previously calculated value of human life results in an estimated economic burden of approximately EUR 1 billion per year, though this figure comes with a substantial uncertainty range (EUR 0.43 billion to EUR 1.67 billion).
Applying this methodology to other types of mortality, such as that associated with respiratory infections, cardiac arrest, or lung cancer, appears feasible as long as the VOLY figure (EUR 43,000) is used. The primary challenge lies in accurately estimating the expected remaining life years at the age of death, which may vary significantly across different ailments compared to the eight years assumed for COVID-19 and heat-related mortality.
5. Conclusions
In this paper, we made an attempt to assess the cost of heat-related mortality by using COVID-19 mortality as a proxy. Our approach focused on Belgium during the first COVID-19 wave (March–June 2020), since this period was exceptionally well documented, and highly accurate daily mortality figures were available. The underlying idea is that the economic losses caused by to the lockdown can be equated to the numerous lives saved due to the lockdown, leading to a unit cost per life saved.
First, it was argued that COVID-19 mortality is indeed a suitable proxy for heat-related mortality. Not only are vulnerable population groups for both COVID-19 and heat nearly identical (elderly people and people with pre-existing disease), the potential number of life years remaining at the age of death is also very similar, being approximately eight years for either.
The monetary cost that can be assigned to a human life under COVID-19 (and by extension, to heat-related mortality) was established by linking the following factors:
- The net loss in the gross domestic product (GDP) occurring in the first half of the year 2020 (i.e., the period encompassing the first COVID-19 wave) due to the measures taken by the government, which was estimated to represent a loss of 19.4 billion ± EUR 2.7 billion;
- The number of avoided deaths due to the lockdown, estimated using evidence from the literature and through epidemiological modelling, considering the hypothetical number of people that were saved due to the measures taken by the government, their number amounting to 52,000 ± 29,000.
The resulting monetary cost of avoiding one death was found to be EUR 377,000 ± EUR 222,000. This amount turns out to be an order of magnitude lower than commonly used values for the Value of a Statistical Life (VSL). Among other things, this was attributed to the relatively short stretch of expected life years remaining at the age of death for extreme heat as compared to all causes of death. As a consequence, when reducing our estimate for the monetary cost of a human life to an annual cost, by dividing by the presumed eight life years remaining at the age of death, the resulting range of EUR 19,000–EUR 75,000 is much closer to the generally accepted values for the Value of a Life Year (VOLY).
The novelty of the approach presented here is that, rather than assessing the cost of a human life based on an individual willingness to pay, it is assessed as an actual collective willingness to pay. This may even be the more appropriate way to go, considering that the cost of climate action and adaptive interventions is borne by collectivity. The main new insight is that our analysis identifies the VOLY, together with a life expectance at the age of death of 8 years, as the preferred approach for quantifying heat-related mortality cost. As mentioned in the Introduction Section, quite some uncertainty regarding the VSL vs. VOLY approach has existed so far; our findings clearly identify the latter as the most appropriate metric.
The relevance and application of these results lie in their utility for supporting cost–benefit assessments of heat-related health climate actions. Mortality cost figures provide critical evidence for decision making, bolstering the case for investments in health protection and serving as a baseline against which the effectiveness of protective measures can be monitored [48]. The significance of these protective measures cannot be overstated. For instance, it has been demonstrated that the heat-related health action plans implemented after the deadly 2003 heatwave in France resulted in a nearly 70% reduction in mortality during the extreme heatwave of 2006 [49]. More recently, an analysis of heat-related mortality in Europe concluded that the death toll during the summer of 2023, which reached nearly 50,000, would have been 80% higher without adaptive actions [50]. Many of these adaptive actions focus on early warning and behavioural changes, which have been found to be highly cost effective; in fact, estimates for France show that the annual operating costs for a heat-related health action plan involves an annual operating cost of EUR 455,000 [21], which is at the same level of cost as that estimated here for a single human life.
This shows that there is ample room to consider additional measures, in particular those targeting infrastructure and urban planning. Urban interventions are not only relevant because of the elevated temperatures occurring in cities, such interventions may also be more efficient considering the high density of people that may benefit from them [51]. One measure that is considered particularly useful in an urban context consists of increasing the abundance of green urban infrastructure [47,52,53]. A study involving 100 European cities [54] has shown that a large potential for additional cooling by greening remains in many cities. While such infrastructural and planning measures are more costly than, e.g., behavioural changes, they bring benefits that last for years or decades. Moreover, urban greening measures bring many other benefits, including a positive impact on the physical and mental health of urban dwellers.
Our analysis has several limitations. First, the number of averted fatalities only accounts for mortality directly associated with COVID-19 infections. It does not account for mortality that might otherwise have been affected by the pandemic, owing to the reduced health care for non-COVID-19 disease, including cancers going undetected and urgent care being postponed [31]. At the same time, the lockdowns have also led to a reduction in certain types of fatalities, such as those related to traffic accidents. Still, balancing all these effects is far from straightforward, which is why they were left out.
Moreover, our approach is limited with respect to the monetary metric used, i.e., net GDP loss, which was used to estimate the amount of wealth a country is prepared to forego to save people from dying. Indeed, other ways to quantify the willingness to pay for a human life (or life year) are available. For instance, the WHO considers a cost per QALY (Quality Adjusted Life Year) of one–three times the GDP per capita as cost-effective [55]. Interestingly, with a Belgian GDP per capita of EUR 43,000 (2019 value), we arrive at a range of EUR 43,000–EUR 129,000 per QALY, suggesting slightly lower values for the VOLY, i.e., not significantly different from our VOLY estimate of EUR 19,000–EUR 75,000.
Finally, the results obtained here cannot easily be transposed to other regions, especially low- or middle-income countries, considering that any pandemic containment measures would probably induce GDP shocks of a different intensity. Also, such countries generally feature a different population age distribution, with a lower share of elderly people, which would affect epidemiological aspects such as the infection fatality rate (IFR). Still, with suitable data regarding actual mortality and net GDP loss, the methodology described in this paper could be replicated to other regions, which will be the subject of future research.
[ad_2]
Source link
Related
Discover more from Mission LiFE
Subscribe to get the latest posts sent to your email.